
Personalized OSA treatment addresses the unique needs of each patient, which has become crucial as the global burden of sleep apnea continues to rise. A recent study revealed that warmer nights increase the likelihood of obstructive sleep apnea by 45%, leading to significant health and economic impacts. Advances in polysomnographic phenotyping, genetic analysis, and integration of AI into clinical practice now enable more precise therapies. These innovations, along with options like CPAP Machines for Sleep Apnea china, help move care beyond traditional, one-size-fits-all approaches and improve patient outcomes.
Key Takeaways
- Obstructive sleep apnea (OSA) affects nearly one billion adults worldwide, making personalized treatment essential to address diverse patient needs.
- Traditional one-size-fits-all OSA treatments often fail due to low patient adherence and lack of consideration for individual differences.
- Advances in genetics, anatomy, and lifestyle understanding help tailor therapies like CPAP, oral appliances, and surgery to each patient’s unique profile.
- Home-based and wearable diagnostic devices improve OSA detection, making testing more accessible and comfortable.
- Early monitoring of therapy use predicts long-term success, so timely support and education boost adherence and outcomes.
- Digital health tools and artificial intelligence enable real-time tracking and personalized adjustments, empowering patients and clinicians.
- Oral appliances suit patients with mild to moderate OSA and specific jaw features, offering a comfortable alternative to CPAP.
- Surgical options target anatomical issues when other treatments fail, requiring careful patient selection and follow-up for best results.
Understanding OSA and the Case for Personalization
OSA Prevalence and Health Impact
Global and regional statistics on OSA
Obstructive sleep apnea (OSA) affects millions worldwide, with prevalence rates rising steadily in both developed and developing regions. Recent estimates suggest that nearly one billion adults globally experience some degree of OSA. In North America, up to 26% of adults may have moderate to severe OSA, while rates in Asia and Europe continue to climb due to aging populations and increasing obesity rates. Urbanization and lifestyle changes contribute to higher incidence in emerging economies. These statistics highlight the urgent need for effective and scalable management strategies.
Health risks of untreated OSA
Untreated OSA poses significant risks to individual and public health. Studies consistently link OSA to increased rates of motor vehicle crashes, likely due to excessive daytime sleepiness and impaired alertness. Some research suggests a possible association with higher all-cause mortality, although the precise mechanisms remain under investigation. While randomized controlled trials have not always demonstrated clear reductions in cardiovascular events or mortality with standard therapies, observational studies indicate that treatment may reduce accident risk and improve symptoms. The Agency for Healthcare Research and Quality emphasizes the need for more robust, long-term studies but cautions against limiting access to therapy, given the clear symptomatic and safety benefits. Persistent symptoms such as excessive daytime sleepiness can severely impact quality of life and daily functioning.
Why Traditional OSA Treatments Are Not Enough
Limitations of standard approaches
Traditional OSA management often relies on the apnea–hypopnea index (AHI) as the primary diagnostic and treatment criterion. This one-size-fits-all approach fails to account for the diverse symptoms, underlying mechanisms, and prognoses seen in OSA patients. Clinical research identifies several key limitations:
- Many patients struggle with adherence to positive airway pressure (PAP) therapy, averaging only 3–5 hours of use per night.
- Trial populations often exclude symptomatic individuals, women, and racially minoritized groups, limiting the generalizability of findings.
- Studies frequently focus on composite cardiovascular outcomes, which can obscure the effects on specific disease subtypes.
- OSA presents with distinct phenotypes and endotypes, similar to conditions like asthma and cancer, which benefit from tailored therapies.
- Emerging diagnostic tools, such as advanced phenotyping and biomarker identification, offer promise but remain complex and not yet practical for routine clinical use.
These factors underscore the need for more personalized, mechanism-based treatment strategies.
The challenge of patient adherence and satisfaction
Patient adherence remains a major barrier to effective OSA management. Early studies found that only about 46% of patients regularly use CPAP for the recommended duration, with average nightly use around 4.7 hours. Adherence rates often range from 30% to 60%, and nonadherence typically develops early and persists over time. Even among those who use therapy consistently, excessive daytime sleepiness can remain prevalent, affecting up to 42% of patients. Higher adherence correlates with improved satisfaction, better relationships, and reduced healthcare costs. However, persistent symptoms and device discomfort can lower satisfaction and lead to treatment discontinuation. These challenges highlight the importance of individualized care models that address both clinical and personal needs, paving the way for more effective and sustainable OSA management in 2025.
The Science of Personalizing OSA Therapy

Individual Factors Shaping OSA Treatment
Genetic and anatomical differences
Genetic and anatomical factors play a central role in shaping both the risk of obstructive sleep apnea (OSA) and the effectiveness of therapy. Twin and family studies reveal that OSA has a strong heritable component, with inheritance rates for OSA-related traits ranging from 30% to over 50%. These genetic influences extend beyond body mass index, age, or gender. For example, the diameter of the oropharynx and tongue volume—both critical anatomical determinants of airway patency—show high heritability. Specific gene polymorphisms, such as those in the ACE gene, have been linked to OSA severity and associated hypertension.
Craniofacial structure also significantly impacts OSA risk and treatment selection. Individuals with smaller mandibular or maxillary bones, a narrower nasopharyngeal airway, or an inferiorly positioned hyoid bone face a higher risk of airway collapse during sleep. Mandibular advancement devices (MADs) often prove effective for patients with these anatomical features, while continuous positive airway pressure (CPAP) remains the standard for many but suffers from low compliance. Muscle function in the tongue, hyoid, and soft palate further influences airway stability, guiding the choice between lifestyle interventions, oral appliances, nerve stimulation, or surgery. Early screening of relatives can help identify those at risk, enabling proactive and personalized prevention strategies.
Lifestyle, behavioral, and ethnic considerations
OSA treatment outcomes depend not only on genetics and anatomy but also on a range of lifestyle, behavioral, and sociodemographic factors. Researchers have identified several key influences:
- Economic status: Individuals with higher income tend to seek treatment earlier and show better acceptance of CPAP therapy. Lower income often leads to treatment delays and higher refusal rates.
- Place of residence: Rural patients experience longer delays in diagnosis and treatment due to limited access to specialized care.
- Family and social support: Strong family ties improve symptom recognition and adherence to therapy. Those living alone often face delays in seeking care.
- Self-recognition of disease: Patients who understand their symptoms tend to seek care more promptly.
- Self-efficacy: Confidence in managing symptoms increases adherence and reduces delays.
- Duration of symptoms: Prolonged snoring, especially over ten years, raises the risk of delayed treatment, often due to stigma or normalization of symptoms.
Additional factors such as age, gender, obesity, and neck circumference also influence OSA risk and therapy response. Older adults and men face higher risk, while obesity and large neck circumference increase the likelihood of pharyngeal collapse. Ethnic differences in craniofacial morphology further affect both disease prevalence and the suitability of specific treatments.
Tip: Identifying these individual factors allows clinicians to select the most appropriate therapy, whether it involves lifestyle changes, oral appliances, nerve stimulation, or surgical intervention.
Advances in Diagnosis and Patient Profiling
Modern sleep studies and home-based testing
Recent technological advances have transformed the landscape of OSA diagnosis. While in-lab polysomnography (PSG) remains the gold standard, a new generation of home-based diagnostic devices now offers greater accessibility and comfort. The American Academy of Sleep Medicine (AASM) classifies these devices into Types II, III, and IV, based on the number and type of sensors used. Type II devices monitor multiple channels, including EEG and respiratory effort, enabling sleep staging and apnea-hypopnea index (AHI) calculation. Type III and IV devices use fewer channels, focusing on heart rate, oxygen saturation, and airflow.
Wearable technologies such as smartwatches and rings equipped with photoplethysmography (PPG), accelerometers, and pulse oximetry have achieved diagnostic accuracies up to 85%. Noncontact methods, including video and audio analysis, have also emerged. For example, video-based systems like SleepWise demonstrate 100% sensitivity and 83% specificity, while sound-based deep learning approaches achieve sensitivities and specificities above 90%. IoT-enabled systems and machine learning algorithms further enhance long-term monitoring and positional sleep apnea detection.
| Device/Method | Sensor Types | Sensitivity | Specificity | Accuracy |
|---|---|---|---|---|
| Medibyte | ECG, Oximetry, Respiratory Effort | 80% | 97% | N/A |
| ApneaLink Plus | Respiratory Effort, Pulse, O2 Sat | N/A | 93% | N/A |
| NOX T3 | Oximeter, Respiratory Inductance | 85% | 89% | N/A |
| Smartwatch (PPG) | Photoplethysmography | N/A | N/A | 85% |
| Belun Ring Platform | O2 Sat, PPG, Accelerometer | 85% | 87% | N/A |
| SleepWise (Video-based) | Video/Image Processing | 100% | 83% | N/A |
| Sound + Deep Learning | Audio | 95.6% | 91.6% | N/A |
| Radio Frequency Radar | Impulse-radio ultra-wideband radar | N/A | N/A | Agreement 0.93 |
| Wearable Nasal Septum System | PPG, Accelerometer | 90% | 90% | N/A |
| IoT-based ECG System | Single-channel ECG | N/A | N/A | 88.2% |
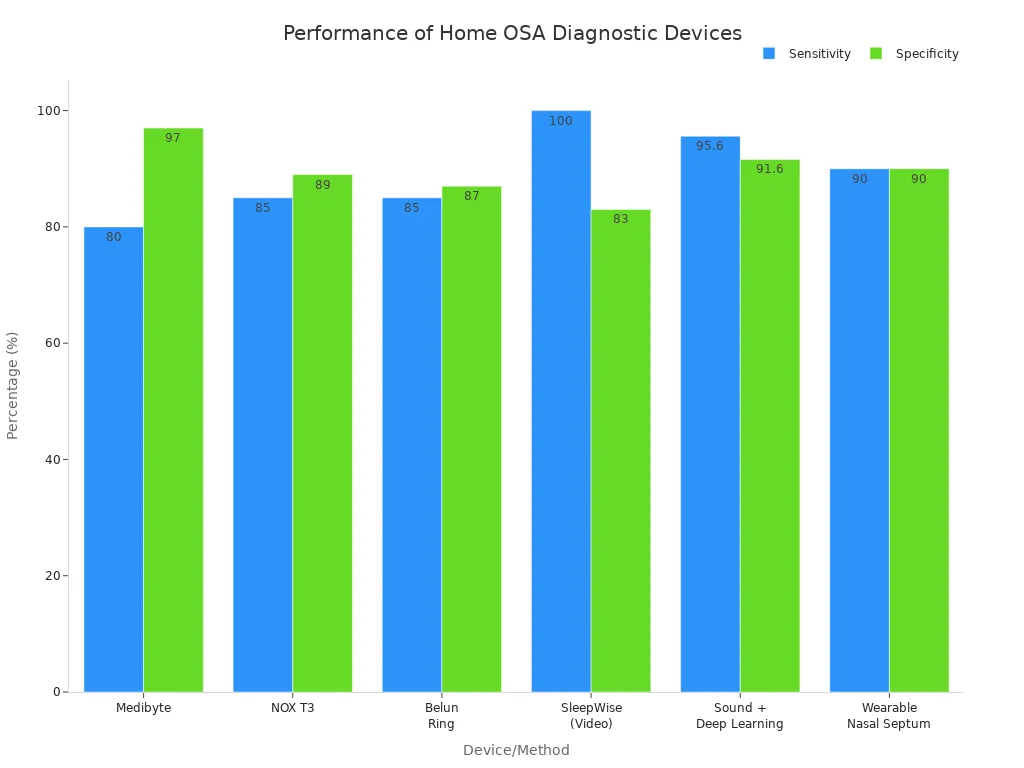
These innovations make OSA diagnosis less invasive and more accessible, but clinical oversight and expert interpretation remain essential for accurate results.
Predictive formulas and algorithms for therapy selection
Clinicians now use advanced computational tools to personalize OSA therapy. Computational 3D models simulate patient-specific airway dynamics, predicting the impact of treatments such as CPAP, oral appliances, or surgery. Cluster analysis and phenotyping help identify OSA subtypes with distinct clinical features and treatment responses. These approaches allow for tailored therapy plans based on individual physiological and clinical characteristics.
Machine learning models predict CPAP compliance and optimize adherence through AI-enabled monitoring systems. Artificial intelligence also forecasts the effectiveness of alternative therapies, such as oral appliances and surgery, supporting clinical decision-making. Integration of computational models with real-time monitoring enables dynamic, adaptive treatment adjustments.
Note: Personalized treatment plans increasingly consider patient preferences, lifestyle, and adherence potential, supported by multidisciplinary clinical teams.
Digital health and remote monitoring innovations
Digital health platforms and remote monitoring technologies have revolutionized OSA management. AI-driven wearable devices collect real-time patient data, enabling clinicians to adjust therapy dynamically. These systems integrate multimodal data, including physiological signals, imaging, and clinical records, to support comprehensive and personalized care.
Remote monitoring tools facilitate early screening, subtype identification, and prognosis evaluation. Machine learning algorithms analyze usage patterns and predict adherence, allowing for timely interventions. These innovations empower patients and clinicians to move beyond one-size-fits-all approaches, delivering more effective and individualized OSA care.
Callout: The integration of digital health and predictive analytics marks a new era in OSA therapy, where precision medicine becomes the standard and every patient receives care tailored to their unique profile.
CPAP Machines for Sleep Apnea china: Personalizing Positive Airway Pressure Therapy

CPAP as the Gold Standard—Strengths and Limitations
Why CPAP is effective for many patients
CPAP Machines for Sleep Apnea china remain the gold standard for treating obstructive sleep apnea. Clinical guidelines and studies confirm that these devices act as pneumatic splints, keeping the upper airway open during sleep. This mechanism eliminates apneas and hypopneas, normalizes oxygen levels, and improves neurocognitive symptoms. Many patients notice better quality of life and reduced daytime sleepiness within weeks of starting therapy. Randomized controlled trials show that CPAP Machines for Sleep Apnea china significantly improve scores on the Epworth Sleepiness Scale and the Sleep Apnea Quality of Life Index, especially for those with moderate to severe OSA. These benefits persist with consistent use, highlighting the importance of adherence.
Barriers to CPAP adherence and comfort
Despite their effectiveness, CPAP Machines for Sleep Apnea china face several barriers to widespread use. Recent patient surveys and clinical observations identify the most common challenges:
- Discomfort with the mask, which can feel restrictive or claustrophobic.
- Improper pressure settings that cause breathing difficulties.
- The time and effort needed for setup, cleaning, and maintenance.
- Lack of noticeable symptom improvement, leading to discouragement.
- Ongoing costs for supplies like filters, masks, and tubing.
- Noise from the machine, which some patients find disruptive.
These issues contribute to national adherence rates of only 30-60% in the first year. Discomfort remains the leading reason for discontinuation, even in pediatric populations. Personalized support, education, and behavioral interventions can help address these barriers.
Customizing CPAP for Individual Needs
Manual versus auto-CPAP titration
Clinicians use both manual and auto-titrating CPAP Machines for Sleep Apnea china to tailor therapy. Manual titration involves overnight monitoring in a sleep lab to find the optimal pressure. Auto-CPAP devices adjust pressure automatically based on detected airway resistance. Both methods aim to maximize comfort and effectiveness, but auto-CPAP offers greater convenience and flexibility for many patients.
Predictive equations for optimal pressure (BMI, SpO2, RDI, Epworth score)
Personalization extends to pressure settings. Clinicians use predictive equations that factor in body mass index (BMI), baseline oxygen saturation (SpO2), respiratory disturbance index (RDI), and Epworth Sleepiness Scale scores. These formulas help estimate the starting pressure for CPAP Machines for Sleep Apnea china, reducing the need for repeated lab visits and improving initial comfort.
Early usage patterns and adherence predictors
Early usage patterns strongly predict long-term adherence. Studies show that most patients establish their CPAP habits within the first two weeks. Those who use CPAP Machines for Sleep Apnea china for at least four hours per night during this period are more likely to remain adherent over months and years. Side effects or discomfort in the first days often lead to lower usage later. Clinicians monitor early patterns and intervene quickly to support patients at risk of non-adherence.
| Early Usage Pattern | Predictive Value | Clinical Implication |
|---|---|---|
| Consistent use | High adherence at 3+ months | Positive long-term outcomes |
| Intermittent use | Lower adherence at 3+ months | Needs early intervention |
| Non-use | Persistent non-adherence | Intensive support required |
Tip: Early identification of low adherence allows for timely interventions, improving long-term outcomes with CPAP Machines for Sleep Apnea china.
Enhancing CPAP Success with Technology and Support
Smart devices and remote monitoring
Technological advances have transformed CPAP Machines for Sleep Apnea china. Modern devices feature comfort enhancements like humidifiers, pressure ramping, and noise reduction. Cloud-based remote monitoring platforms, such as AirView, allow clinicians to track usage data in real time. Patient engagement tools, including mobile apps like myAir and SleepMapper, provide personalized feedback, coaching, and reminders. These innovations increase average nightly use and help more patients meet adherence goals.
Patient education and behavioral interventions
Education and behavioral support play a crucial role in successful therapy. Clinicians assess patient readiness, beliefs, and expectations to tailor education. Shared decision-making and motivational techniques address individual concerns. Teach-back methods and personalized coaching improve self-efficacy, which predicts better use of CPAP Machines for Sleep Apnea china. Virtual setups and instructional videos, especially during the COVID-19 pandemic, have proven as effective as traditional face-to-face education. These strategies empower patients and foster long-term adherence.
Oral Appliances: Matching Devices to Patient Profiles
Mechanism and Suitability of Oral Appliances
How mandibular advancement works
Oral appliance therapy (OAT) offers a noninvasive approach to treating obstructive sleep apnea. The most common devices, mandibular advancement devices (MADs), function by moving the lower jaw forward. This anterior displacement increases the cross-sectional area of the upper airway, especially in the velopharyngeal region. By enlarging this space, MADs reduce the likelihood of airway collapse during sleep. The pharyngeal airway, which lacks rigid skeletal support, becomes less prone to obstruction when the jaw and tongue shift forward. Some devices, such as tongue-retaining devices, also exist, but patients often tolerate them less well due to retention issues.
Note: Custom-made, titratable MADs provide better comfort and efficacy compared to prefabricated or non-adjustable options.
Suitability for different craniofacial features and populations
Not every patient responds equally to oral appliance therapy. Several traits predict better outcomes:
- Mild-to-moderate OSA severity
- Supine-predominant OSA
- Younger age and female gender
- Lower body mass index (BMI) and neck circumference
- Craniofacial features such as a retrognathic (recessed) mandible
- Milder pharyngeal collapsibility and tongue base collapse
Patients with these characteristics often experience greater improvements. Some individuals with severe or overweight profiles may also benefit, but results vary. Imaging studies and drug-induced sleep endoscopy help clinicians identify suitable candidates by visualizing airway changes with simulated jaw advancement.
Predicting and Optimizing Oral Appliance Success
The role of the remotely controlled mandibular positioner (RCMP)
The remotely controlled mandibular positioner (RCMP) has emerged as a valuable tool for optimizing oral appliance therapy. During sleep studies, clinicians use the RCMP to adjust the jaw position in real time. This process helps determine the optimal degree of mandibular advancement needed to maintain airway patency. By simulating the effects of an oral appliance, the RCMP allows for precise customization before device fabrication.
Predictive values and candidate selection
Clinicians rely on several methods to predict oral appliance success:
- Drug-induced sleep endoscopy (DISE) evaluates upper airway obstruction. A jaw thrust maneuver during DISE simulates the effect of a MAD. Patients who show significant airway improvement at the velum and oropharynx are considered good candidates.
- Visualization of the arytenoids and at least two-thirds of the true vocal folds, along with an estimated airway increase of 3 mm or more, signals likely benefit.
- Clinical variables such as age, BMI, apnea-hypopnea index (AHI), and polysomnography data guide selection.
- Patient preference and intolerance to positive airway pressure therapy also influence the decision.
The American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine recommend that licensed dentists fabricate custom oral appliances for optimal results.
Long-Term Outcomes and Considerations
Efficacy in symptom reduction and quality of life
Mandibular advancement devices improve quality of life, reduce daytime sleepiness, and enhance sleep quality for many patients with mild to moderate OSA. Studies show that, while CPAP reduces the apnea-hypopnea index more effectively, MADs often achieve similar improvements in sleepiness and daily functioning. Patient satisfaction and adherence rates tend to be higher with oral appliances.
Cost-effectiveness and long-term health impacts
Oral appliance therapy can lower healthcare costs by reducing OSA-related comorbidities and accidents. Improved adherence and patient preference contribute to these savings. Some evidence suggests that MADs offer a cost-effective alternative to CPAP, especially in moderate OSA cases. Ongoing research, including large multi-center trials, aims to clarify the long-term cardiovascular and mortality benefits of OAT.
Importance of correct use and follow-up
Proper use and regular follow-up are essential for sustained success with oral appliances. Licensed dentists should monitor patients for device fit, dental changes, and symptom control. Long-term side effects are generally mild, such as minor dental occlusion changes. Consistent follow-up ensures continued efficacy and addresses any emerging issues, supporting better health outcomes over time.
Tip: Patients who choose oral appliance therapy should schedule regular dental and sleep medicine visits to maximize benefits and minimize risks.
Surgical Interventions: When and How to Personalize
Indications and Patient Selection for OSA Surgery
Anatomical abnormalities and therapy failure
Surgical intervention becomes a consideration when patients with obstructive sleep apnea do not respond to or cannot tolerate device-based therapies, such as CPAP. Anatomical abnormalities, including nasal deformities, enlarged tonsils, or skeletal deficiencies, often drive the decision for surgery. A thorough preoperative assessment includes clinical history, physical examination, and formal sleep studies. Physicians use validated questionnaires, such as the Epworth Sleepiness Scale and STOP-Bang, to evaluate symptom burden and predict surgical outcomes. Anatomical evaluation tools, like the Mallampati score and flexible nasopharyngolaryngoscopy, help identify the specific sites of airway obstruction. Multilevel obstruction is common, so a multidisciplinary approach ensures that surgical plans address all relevant anatomical factors.
Criteria for surgical candidacy
Clinicians select surgical candidates based on several criteria:
- Failure or intolerance of CPAP or oral appliance therapy.
- Patient preference for surgery after comprehensive counseling.
- Favorable anatomy identified during examination.
- Absence of significant comorbidities that would increase surgical risk.
- Realistic expectations regarding outcomes and risks.
Patient counseling remains essential. Surgeons must discuss the adjunctive or curative nature of surgery, possible risks, and the likelihood of needing additional therapies.
Types of Surgical Procedures
Nasal surgeries (septoplasty, turbinate reduction)
Nasal surgeries, such as septoplasty and turbinate reduction, improve nasal airflow and can enhance CPAP compliance. These procedures rarely cure OSA but often reduce the pressure required for effective CPAP therapy.
Oral and palatal surgeries (tonsillectomy, uvulopalatopharyngoplasty)
Tonsillectomy and adenoidectomy serve as first-line treatments for children with OSA, achieving cure rates of 60% to 80%. In adults with tonsillar hypertrophy, these surgeries can reduce the apnea-hypopnea index by about 65%. Uvulopalatopharyngoplasty (UPPP) remains the most common surgery for adults with soft palate obstruction. UPPP removes excess tissue from the soft palate and pharynx, with success rates ranging from 33% to 50%. Palatal implants offer a minimally invasive option for mild OSA and snoring.
Hypopharyngeal and tongue-base procedures
Procedures targeting the tongue base, such as radiofrequency ablation, reduction glossectomy, and transoral robotic surgery, address tongue-related obstruction. These interventions suit patients with mild-to-moderate OSA who cannot tolerate CPAP. Success rates vary, with transoral robotic surgery showing the highest efficacy among these options.
Maxillomandibular advancement (MMA) and its role in specific populations
Maxillomandibular advancement (MMA) is reserved for severe or refractory OSA, especially in patients with skeletal abnormalities. MMA advances both the upper and lower jaws, significantly enlarging the airway. This procedure achieves high success rates, around 87%, but results in noticeable facial changes. MMA is most appropriate for patients who have failed other treatments or have clear maxillomandibular deficiency.
Outcomes, Risks, and Recovery
Success rates and patient profiles
Surgical outcomes depend on the type of procedure, patient anatomy, and severity of OSA. Children respond best to tonsillectomy and adenoidectomy. Adults with isolated soft palate obstruction may benefit from UPPP or palatal implants. Patients with multilevel or skeletal obstruction often require MMA. Hypoglossal nerve stimulation offers a less invasive alternative for select patients.
Risks, recovery, and long-term follow-up
OSA patients face higher risks of postoperative respiratory and cardiovascular complications. Respiratory events, such as rapid oxygen desaturation, occur more frequently in this group. Careful perioperative management, including optimal patient positioning and use of positive airway pressure devices, reduces these risks. Despite increased respiratory events, studies show no significant difference in hospital length of stay or readmission rates between OSA and non-OSA patients when managed appropriately.
| Aspect | Findings |
|---|---|
| Postoperative Respiratory Events | Higher in OSA patients (13-15%) vs moderate risk (2.2%) |
| Use of Postoperative Respiratory Devices | 49% of diagnosed OSA patients used devices post-op |
| Length of Stay | No significant difference between groups |
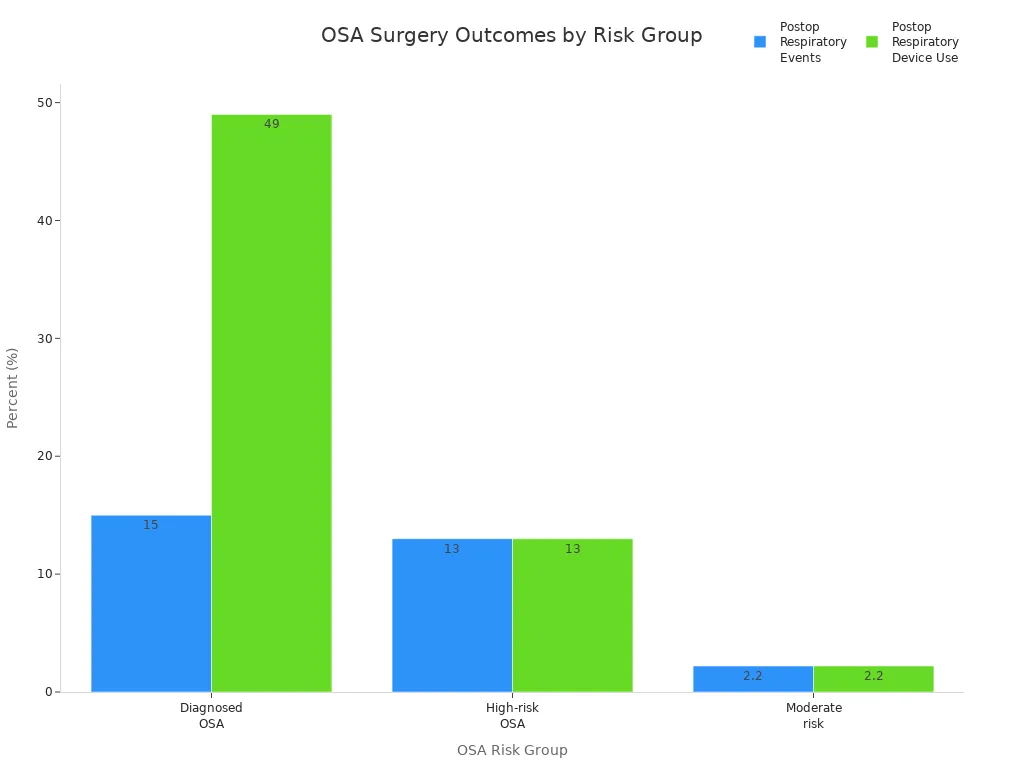
Regular follow-up ensures early detection of complications and long-term success. Personalized surgical plans, tailored perioperative care, and patient education remain key to optimizing outcomes in OSA surgery.
Novel and Adjunctive Therapies: Expanding the Personalized Toolbox
Upper Airway Muscle Training
The science behind muscle dysfunction in OSA
Upper airway muscle dysfunction plays a significant role in the development of obstructive sleep apnea. Poor responsiveness of these muscles contributes to airway collapse in at least 30% of patients. The patency of the upper airway depends on the coordinated activity of dilator muscles such as the genioglossus and sternohyoid. When these muscles fail to activate properly during sleep, the airway narrows and collapses more easily. Sedentary lifestyles can worsen this problem by promoting fluid retention in the legs, which shifts to the neck during sleep and increases airway compression.
Evidence for oropharyngeal exercises and tongue training
Oropharyngeal exercises and tongue training have emerged as promising interventions. Clinical studies show that upper airway muscle training can reduce the apnea-hypopnea index (AHI) by nearly 50%, improve oxygen saturation, and decrease daytime sleepiness. Respiratory muscle training, which involves breathing against resistance, strengthens inspiratory and expiratory muscles. Myofunctional therapy targets oral and oropharyngeal muscles, leading to better muscle tone and reduced airway collapsibility. Animal studies also suggest that endurance exercise induces beneficial changes in upper airway muscle fibers.
Tip: Patients who engage in regular exercise may see additional benefits, as increased respiratory muscle recruitment enhances upper airway stability.
Identifying patients who benefit most
Not all patients respond equally to muscle training. Those with poor upper airway muscle responsiveness or anatomical predispositions to airway collapse tend to benefit the most. Individuals with sedentary behavior and fluid accumulation in the neck may also experience improvements through exercise. Personalized training regimes and further research are needed to optimize outcomes and identify the best responders.
Hypoglossal Nerve Stimulation
How the implantable device works
Hypoglossal nerve stimulation (HNS) uses an implantable device to activate the hypoglossal nerve, which controls tongue movement. By stimulating this nerve during sleep, the device increases upper airway muscle tone and reduces airway collapse.
Patient selection and clinical outcomes
| Aspect | Details |
|---|---|
| Clinical Evidence | Long-term studies, such as the STAR trial, show sustained reductions in AHI and improved quality of life. |
| Key Inclusion Criteria | Moderate to severe OSA (AHI 15–65), BMI <32 kg/m², absence of complete concentric collapse at the soft palate, and CPAP intolerance or failure. |
| Exclusion Criteria | Central sleep apnea >25%, positional OSA, large tonsils, tongue malformations, neuromuscular disease, psychiatric illness, pregnancy, or other implantable devices. |
| Additional Considerations | Psychological readiness and motivation are critical. Post-operative titration and follow-up optimize outcomes. Cost remains a significant factor. |
HNS can reduce AHI by up to 70% in selected patients, but about one-third may not respond. Personalized assessment and comprehensive management improve success rates.
Risks and considerations
HNS implantation carries surgical risks, including infection and device malfunction. Not all patients qualify, and the high cost limits widespread use. Careful patient selection and ongoing follow-up are essential for safety and efficacy.
Other Emerging Therapies and Lifestyle Interventions
Neuromuscular electrical stimulation
Neuromuscular electrical stimulation targets weak oropharyngeal muscles to increase tone and reduce airway collapsibility. Early studies suggest potential benefits, especially for patients with poor muscle responsiveness.
Hyperbaric oxygen and other alternatives
Supplemental oxygen therapy can help patients with high loop gain by stabilizing ventilatory control and reducing AHI by up to 50%. Hypnotic agents may increase arousal thresholds, but clinicians must use caution in severe cases.
The role of weight loss and exercise
Weight loss remains a cornerstone of OSA management. Reducing pharyngeal fat decreases airway collapsibility and improves patency. Regular exercise not only aids weight loss but also enhances upper airway muscle function and fluid dynamics, offering additional benefits for sedentary individuals.
Note: Personalized OSA management now combines phenotyping, targeted therapies, and lifestyle interventions to improve outcomes and patient adherence.
Real-World Outcomes and Ongoing Research
Evidence from Clinical Trials and Studies
Success rates across different therapies
Recent clinical trials have revealed that personalized OSA therapies can produce highly variable outcomes, depending on patient characteristics. In adults with nonsleepy OSA and acute coronary syndrome, researchers used machine learning to identify subgroups with different responses to CPAP therapy. Patients with shorter apnea event durations (19.5 seconds or less) experienced fewer cardiovascular events when treated with CPAP. However, those with longer events and high cholesterol faced increased cardiovascular risk with the same therapy. These findings highlight the complexity of OSA and the need for individualized treatment strategies based on accessible clinical metrics, such as apnea duration and cholesterol status.
In pediatric OSA, new studies focus on tailoring surgical approaches using drug-induced sleep endoscopy (DISE). DISE helps surgeons pinpoint the exact site of airway obstruction, moving beyond the standard adenotonsillectomy. Early data show that DISE ratings align closely with OSA severity and predict surgical outcomes more accurately than traditional tonsil size assessments. Personalized surgery based on DISE may improve results and reduce unnecessary procedures, especially for children with small tonsils. However, most current studies remain small and lack direct randomized comparisons, so further research is needed.
Gaps in research and the need for diverse populations
- Significant disparities exist in OSA treatment among older adults with neurological disorders. Women and racial or ethnic minorities show lower rates of CPAP treatment and adherence.
- A large Medicare study found that only 73% of patients received CPAP, with even lower rates among those with neurological conditions such as stroke, cognitive disorders, and Parkinson’s disease.
- Gender and race influence the likelihood of receiving and adhering to OSA therapy, with women and minorities at a disadvantage.
- Stroke patients have the lowest treatment and adherence rates, despite the high prevalence of sleep apnea after ischemic stroke and its link to poor recovery.
- Barriers include underdiagnosis, unclear timing for intervention, and lack of clear guidelines, especially for non-Hispanic white populations who are more likely to receive treatment.
- There is a critical need for multidisciplinary strategies and more research on long-term outcomes in these vulnerable groups.
Note: Addressing these gaps will require targeted outreach, culturally sensitive care, and improved access to diagnostic and therapeutic resources.
The Importance of Long-Term Follow-Up
Monitoring health outcomes beyond OSA indices
Long-term follow-up plays a vital role in assessing the true effectiveness of personalized OSA treatments. A 10-year study of patients using CPAP or mandibular advancement devices (MAD) showed that both therapies maintained improvements in apnea-hypopnea index (AHI), oxygen saturation, and self-reported outcomes. However, AHI gradually increased over time, likely due to aging and anatomical changes. Many patients discontinued or switched therapies, which underscores the need for regular monitoring of adherence and effectiveness.
Objective sleep studies every few years help verify ongoing treatment success, as self-reported outcomes often overestimate actual benefits. Long-term side effects, such as dental changes from MAD therapy, may require adjustments. Aging also increases airway collapsibility, which can reduce treatment effectiveness.
Integrating patient feedback and quality of life measures
Clinicians must look beyond sleep study numbers to evaluate patient well-being. Quality of life, daytime alertness, and satisfaction with therapy provide essential insights into treatment success. Regular feedback helps clinicians adapt therapy to changing needs and address emerging issues. Only a minority of patients complete long-term follow-up, so repeated assessments and patient engagement remain crucial for sustained success.
Tip: Ongoing communication and periodic reassessment ensure that personalized OSA therapies continue to meet each patient’s evolving needs and deliver lasting health benefits.
The Future of Personalized OSA Care
Integrating Technology and Data for Precision Medicine
Artificial intelligence and machine learning in OSA management
Artificial intelligence (AI) and machine learning are transforming the landscape of OSA management. These technologies analyze large datasets from sleep studies, wearable devices, and electronic health records to identify patterns and predict treatment outcomes. AI-driven models can forecast which patients will benefit most from specific therapies, such as CPAP or oral appliances. Machine learning algorithms also help clinicians recognize high-risk individuals and anticipate complications, supporting proactive care.
- Multi-night home sleep monitoring devices allow patients to undergo testing in their own homes, capturing data over several nights and improving diagnostic accuracy.
- Advanced signal processing techniques extract new markers like ventilatory burden and hypoxic burden, offering deeper insights than traditional metrics.
- Smart oral appliances now include sensors that track temperature, oxygen saturation, heart rate, and sleep stages, providing real-time feedback for both patients and clinicians.
- Cloud-based platforms enable seamless data sharing among dentists, sleep physicians, and patients, supporting continuous monitoring and timely adjustments.
- AI-powered decision support systems integrate with electronic health records, guiding personalized anesthesia planning and perioperative management for OSA patients.
Patient engagement tools, such as mobile apps and telemedicine, deliver personalized education and reminders, which enhance adherence and empower individuals to take an active role in their care.
The promise of digital health platforms
Digital health platforms have become central to precision medicine in OSA care. These platforms connect patients and providers, streamline data collection, and facilitate remote monitoring. Wearable devices track sleep patterns, oxygen levels, and vital signs, enabling early detection of problems and timely interventions. Telemedicine expands access to care, especially in underserved communities, by allowing virtual consultations and follow-up visits.
Remote monitoring systems for positive airway pressure (PAP) therapy have already improved adherence rates. Similar platforms for oral appliances are under development, promising to extend these benefits. Data analytics help clinicians evaluate treatment effectiveness and identify opportunities for quality improvement. As technology advances, digital health platforms will continue to drive more personalized, efficient, and accessible OSA care.
Moving Toward Patient-Centered OSA Treatment
Shared decision-making and individualized care plans
Patient-centered OSA care emphasizes shared decision-making and individualized treatment plans. Clinicians now recognize OSA as a heterogeneous disease, requiring therapies tailored to each patient’s unique physiological traits and lifestyle. The integration of multidisciplinary teams—including sleep physicians, dentists, and behavioral specialists—ensures that care addresses both medical and personal needs.
| Aspect | Evidence Supporting Patient-Centered OSA Treatment Trends and Future Directions |
|---|---|
| Current Trends | Shift toward precision medicine, use of wearable devices, multidisciplinary approaches, and recognition of OSA heterogeneity. |
| Future Directions | Standardized tools for trait assessment, patient-centered outcome studies, expanded research in diverse populations, and non-invasive treatments. |
| Clinical Implications | Personalized plans based on pathophysiological traits, multidisciplinary teams, and new adjunct therapies to improve adherence. |
| Challenges | Need for better trait-phenotype understanding, technology adoption barriers, and ensuring equitable access. |
Clinicians and patients work together to select therapies that align with individual goals, preferences, and daily routines, improving satisfaction and long-term outcomes.
The evolving role of primary care and multidisciplinary teams
Primary care providers and multidisciplinary teams play a growing role in the future of OSA management. They coordinate care across specialties, ensuring that patients receive comprehensive evaluation and follow-up. Collaboration among technologists, clinicians, and patients drives innovation and supports the adoption of new technologies. As non-invasive, home-based monitoring devices become more common, primary care teams will help guide patients through diagnosis, therapy selection, and ongoing management.
The future of personalized OSA care depends on continued research, patient education, and equitable access to advanced diagnostics and therapies. By embracing technology and fostering collaboration, healthcare teams can deliver more effective, patient-centered solutions for individuals living with OSA.
Personalized OSA treatments in 2025 deliver patient-centered care by matching therapies to individual needs. Scientific advances and digital health tools drive better outcomes and higher satisfaction. Studies show that:
- Adherence to positive airway pressure therapy improves quality of life scores.
- Continuous PAP treatment reduces daytime sleepiness and lowers the risk of motor vehicle accidents.
- Therapy addresses depression by improving sleep quality and reducing neuroinflammation.
Neuroimaging research reveals that tailored OSA therapy can reverse brain structural damage and enhance cognitive function. Ongoing studies use digital technology to improve adherence and address health disparities, especially in underserved populations. Patients experience improved quality of life, reduced health risks, and greater empowerment throughout their treatment journey.
FAQ
What makes OSA treatment “personalized” in 2025?
Personalized OSA treatment uses genetic, anatomical, and lifestyle data to match therapies to each patient. Clinicians select interventions based on individual characteristics, not just standard protocols.
How do digital health tools improve OSA management?
Digital health platforms track therapy use, symptoms, and sleep patterns. Clinicians review this data remotely and adjust treatment quickly. Patients receive feedback and reminders, which support better adherence.
Who benefits most from oral appliance therapy?
Patients with mild to moderate OSA, smaller jaw structures, or intolerance to CPAP often benefit most. Dentists assess craniofacial features and airway anatomy before recommending oral appliances.
Are surgical options safe for all OSA patients?
Surgical interventions suit patients with specific anatomical issues or failed noninvasive therapies. Surgeons evaluate risks, comorbidities, and airway structure before recommending surgery.
Can wearable devices diagnose OSA accurately?
Wearable devices now achieve up to 85% diagnostic accuracy. They monitor oxygen levels, heart rate, and sleep position. Clinicians confirm results with formal sleep studies when needed.
What role does weight loss play in OSA treatment?
Weight loss reduces airway fat and improves muscle function. Many patients see significant symptom improvement with even modest weight reduction. Exercise also enhances upper airway stability.
How often should patients follow up after starting OSA therapy?
Regular follow-up visits, especially in the first year, help monitor adherence, side effects, and therapy effectiveness. Ongoing assessments ensure that treatment remains optimal as patient needs change.
Is artificial intelligence used in OSA care today?
Clinicians use AI to analyze sleep data, predict therapy success, and identify patients at risk for poor adherence. AI-driven tools support decision-making and personalize care plans.
Post time: Jul-30-2025